DCMWC Transfer Outstanding Debts to CRS
Effective August 24, 2024, the Division of Coal Mine Workers’ Compensation (DCMWC) will initiate a recoupment process in conjunction with the Treasury Department to recover outstanding provider debts owed to the Federal Black Lung Program.
Currently, the Federal Black Lung Program automatically recoups the full amount owed from current and future provider payments until the debt is paid in full.
On or after August 24, 2024, if the debt remains unpaid after 120 days from the Remittance Voucher (RV) overpayment notice, the account balance will be sent to the Centralized Receivables Service (CRS) for collections.
If you have an inquiry or concern regarding the Remittance Voucher (RV) overpayment notice, please submit the RV overpayment notice and all supporting documentation to the following address:
Division of Coal Miner Workers’ Compensation (DCMWC)
General Correspondence
P.O. Box 8307
London, Kentucky 40742-8307
For questions, contact our Call Center at the phone number listed below, where a Call Center representative will be happy to assist you.
Division of Coal Mine Workers' Compensation (DCMWC): 1-800-638-7072
OWCP adjustment/void processing for DFEC and DCMWC
Effective June 1, 2024, the Office of Workers’ Compensation Programs (OWCP) will implement updates for adjustment/void processing.
For the Division of Federal Employees’ Compensation (DFEC), providers will no longer be allowed to submit bill void transactions.
- Providers wishing to return funds have the option to mail the refund along with an Adjustment Request template as the coversheet.
- For assistance in viewing the PDF, please select this link: How to view PDFs using Adobe Reader
For the Division of Coal Mine Workers’ Compensation (DCMWC), providers will have the new option to submit bill adjustments using the WCMBP portal.
- You may refer to the Bill Adjustment tutorial for further information.
For the Division of Energy Employees Occupational Illness Compensation (DEEOIC), there are no changes in the current process for adjustment requests.
For questions, contact our Call Center at the applicable phone number listed below, where a Call Center representative will be happy to assist you.
Division of Coal Mine Workers' Compensation (DCMWC):
1-800-638-7072
Division of Energy Employees Occupational Illness Compensation (DEEOIC):
1-866-272-2682
Division of Federal Employees' Compensation (DFEC):
1-844-493-1966
New Benefit Cards (DEEOIC and DCMWC claimants)
If you are a DEEOIC or DCMWC claimant, you will be receiving a new benefits card in the mail in March 2024 with associated documents from Acentra Health on behalf of OWCP. Your current card will remain active until March 15, 2024. If you do not receive your card by March 15, 2024, please call Acentra Health Customer Service toll-free number for DCMWC at 1-800-638-7072 or DEEOIC at 1-866-272-2682.
Announcement of DEEOIC and DCMWC Pharmacy Benefit Program
The U.S. Department of Labor (DOL) has contracted with myMatrixx®, an Express Scripts Company, to provide Pharmacy Benefit Management (PBM) services to the Office of Workers’ Compensation Programs (OWCP) Division of Energy Employees Occupational Illness Compensation (DEEOIC) and Division of Coal Mine Workers’ Compensation (DCMWC).
All DEEOIC and DCMWC claimants should now have new Medical Benefit Identification Cards (MBIC) and access to myMatrixx®’s nationwide network of participating pharmacies and durable medical equipment. If you are a DEEOIC or DCMWC claimant and still need a new MBIC, please contact the CNSI customer service toll-free number at 1-800-638-7072 for DCMWC or at 1-866-272-2682 for DEEOIC.
Claimants can search for participating pharmacies on the web or by calling myMatrixx®:
- DCMWC - https://blacklung-pharmacy.dol.gov/ or 1-877-880-9215
- DEEOIC - https://energyworkers-pharmacy.dol.gov/ or 1-866-686-9592
As of June 5, 2023, pharmacies have been required to submit their pharmacy transactions to myMatrixx® for payment. Pharmacy providers are encouraged to join the myMatrixx® network and can enroll at www.esiprovider.com.
Medical Providers – Effective May 13, Supporting Medical Documentation Required!
Effective May 13, 2023, the Division of Coal Miner Workers’ Compensation Program (DCMWC) will require medical providers and facilities to submit supporting medical documentation for services they provide to claimants for their covered black lung conditions. You must attach supporting medical documentation when you submit a Health Care Finance Administration form (HCFA-1500) for professional services rendered in a physician’s office, or a Uniform Medical Billing form (UB-04) for all hospital services except non-emergency services of 24 hours or less (for which you may use either form).
The provider submitting the reimbursement form is responsible for attaching sufficient supporting documentation to substantiate the medical services or supplies billed. The supporting documentation must be attached to the bill submission and must support the billing codes submitted on the reimbursement form. All medical services provided to DCMWC claimants must be documented in the submitted supporting documentation, including the date of service, the miner’s name and date of birth, and a signature of the rendering provider that is both legible and time/date stamped.
More information on how to upload and submit bills and attachments through the Workers Compensation Medical Bill Portal’s Direct Data Entry function is available at https://owcpmed.dol.gov/. This link also has training tutorials to help you get familiar with the entire process.
Please review examples of required supporting documentation that should be attached to bills. For additional details please refer to our letter to enrolled providers.
If you have any questions, regarding the contents of this letter, please contact DCMWC’s medical bill processing vendor at 1-800-638-7072.
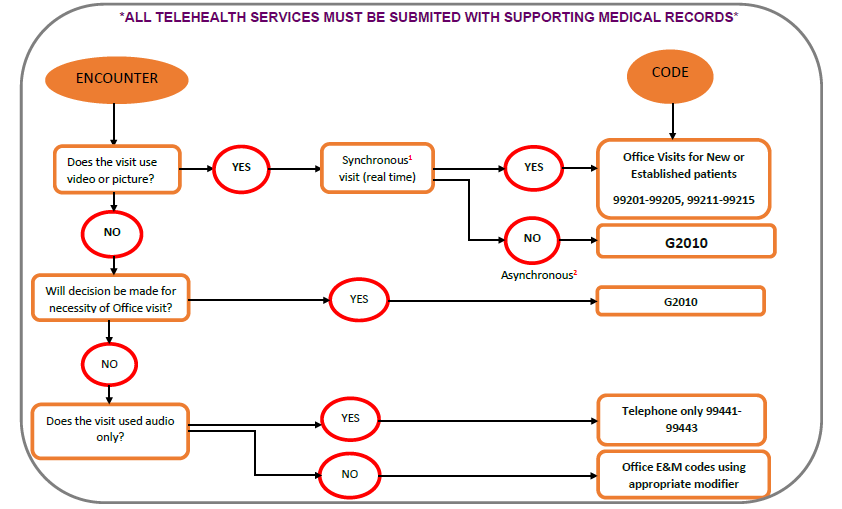
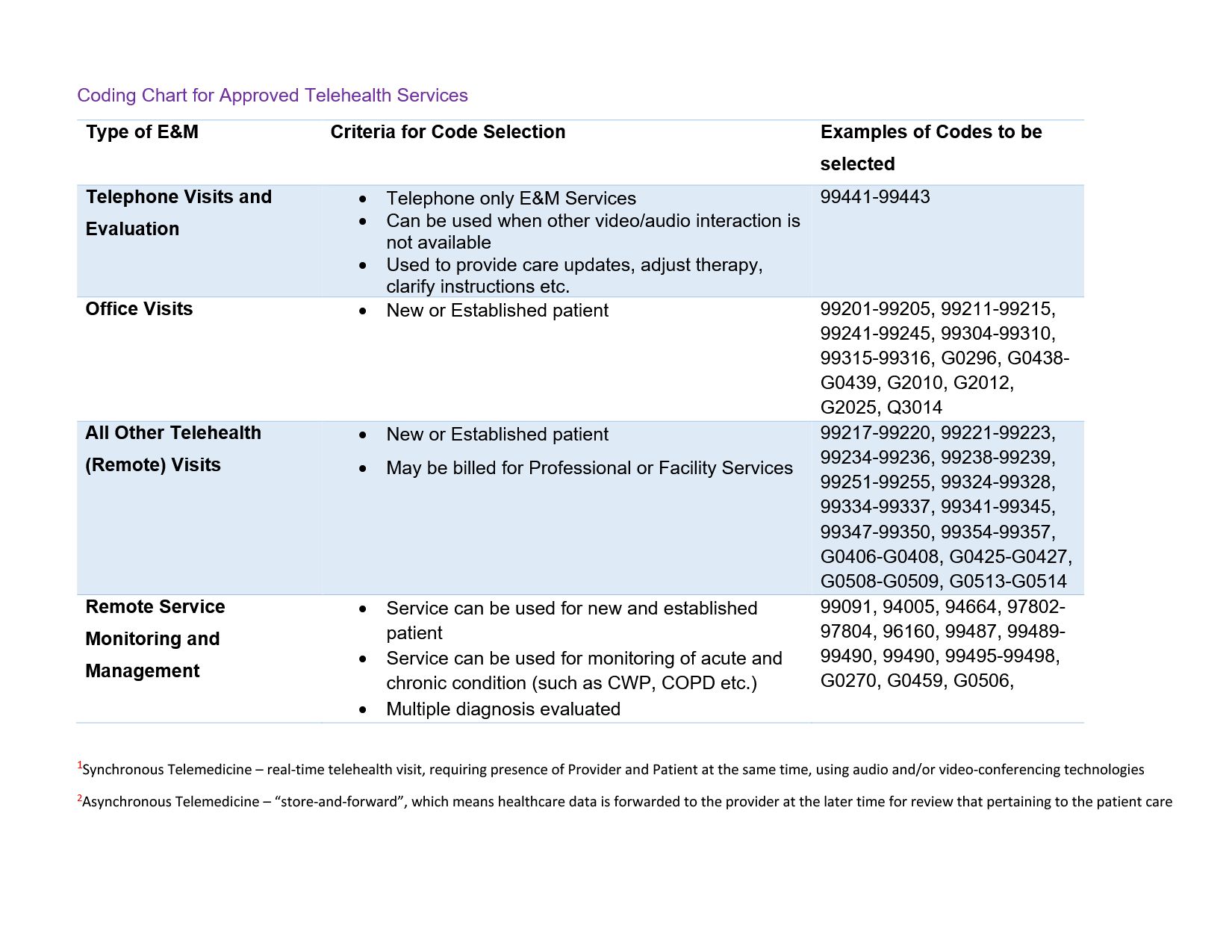
TELEHEALTH BILLING GUIDANCE
TELEHEALTH BILLING GUIDANCE is presented by the DCMWC to assist providers in understanding acceptable billing codes for telehealth services as they relate to the Black Lung program. Click here for additional information regarding DCMWC telehealth guidelines.
Important Notice Concerning Coverage of Lung Transplants by the Federal Black Lung Program
The Division of Coal Mine Workers' Compensation, or Federal Black Lung Program, requires prior approval of the pre-transplant evaluation for lung transplants and the lung transplant itself for Black Lung beneficiaries (20 C.F.R. § 725.705).
Information about an individual's general eligibility for medical benefits may be obtained by calling the District Office where the patient's claim file is located, or by calling the Black Lung toll-free number at (800) 638-7072. Eligibility for medical benefits does not automatically include approval for a pre-transplant evaluation or a lung transplant.
Before seeking approval for a pre-transplant evaluation or a lung transplant, a medical center must be approved as a lung transplant center by the Center for Medicare and Medicaid Services (CMS), or the request will automatically be denied. The list of approved transplant centers is available at:
https://qcor.cms.gov/default.jsp?referer=http://qcor.cms.gov/main.jsp
After reaching the homepage, select the “Resources” link on the upper right hand of the page. A pop-up window will open. Select link for “List of CMS-Approved Organ Transplant Programs”. This will open an excel spreadsheet which contains certification information for all Medicare-certified transplant programs, organized by State. Please refer to the approved lung transplant programs.
Approved lung transplant centers must determine if the patient's medical benefits are the responsibility of a coal mine operator or insurer or the Black Lung Disability Trust Fund. The patient should have this information. For a pre-transplant evaluation or transplant to be considered, it must be necessitated by the coal miner's black lung condition and directly related conditions. If the patient is covered by an insurer or coal mine operator, the company's approval must be obtained prior to a pre-transplant evaluation or transplant. Pre-transplant evaluation and transplant coverage is decided on a case-by-case basis. The Federal Black Lung Program expects coal mine operators or insurers to provide the same coverage that it does. The documentation that coal mine operators or insurers require to determine whether or not they will approve coverage may vary.
If the patient is covered by the Black Lung Disability Trust Fund, the approval process must be initiated by emailing the request to https://owcpmed.dol.gov or by calling the toll-free number (800) 638-7072.
Requests for pre-transplant evaluations and lung transplants should include basic information including the patient's name and date of birth, as well as the name of the facility performing the evaluation or transplant.
Additionally, a request for a pre-transplant evaluation must include a physician's letter of justification. A physician's letter of medical justification is a well-rationalized narrative statement, prepared by a qualified physician who has been actively treating the patient for their pulmonary condition. The letter of medical justification represents the physician's independent assessment and opinion and must include a brief review of the claimant's pertinent medical history, a brief statement regarding the claimant's current medical condition, and explanation of the claimant's medical need for a lung transplant evaluation.
Requests for lung transplants must include the medical facility's lung transplant protocols and all medical records produced for the pre-transplant evaluation, including the results of all tests, consultations, and narrative reports.
After the Federal Black Lung Program evaluates the information submitted, it will notify the requestor of a determination regarding coverage. Any pre-transplant evaluation or transplant performed prior to receiving prior approval by the Federal Black Lung Program will be denied.
Any questions about pre-transplant evaluations or transplants should be directed to the Division of Coal Mine Workers' Compensation at efax-maos-transplant@dol.gov or by calling the toll-free number (800) 347-2502.
ANNOUNCEMENT CONCERNING IN-FACILITY PULMONARY REHABILITATION SERVICES FOR BLACK LUNG BENEFICIARIES
Effective January 1, 2022, in accordance with guidance set forth by the Centers for Medicare and Medicaid Services (CMS), DCMWC introduced two new pulmonary rehabilitation procedure codes, 94625 and 94626, to be billed for pulmonary rehabilitation services.
Effective July 1, 2022, the Healthcare Common Procedure Coding System (HCPCS) pulmonary rehabilitation procedure code G0424, will no longer be covered.
Please note that DCMWC will not pay for at-home pulmonary rehabilitation services.
Preauthorization is not required for in-facility pulmonary rehabilitation services.
Pulmonary rehabilitation providers must be enrolled in the DCMWC provider network to treat miners and receive payment for services. To enroll as a DCMWC provider, please access: the Web Bill Processing Portal<https://owcpmed.dol.gov/portal/> for enrollment instructions.
All bills for pulmonary rehabilitation services must be submitted on the OWCP-1500 claim form. A downloadable OWCP-1500 form<https://www.dol.gov/sites/dolgov/files/owcp/dfec/regs/compliance/owcp-1500.pdf> is available. Providers must use current procedure codes 94625 and 94626 when billing for pulmonary rehabilitation services. A bill for pulmonary rehabilitation services must include at least one of the following mandatory components:
1. Physician-prescribed exercise;
2. Education or training;
3. Psychosocial assessment;
4. Outcome's assessment; or
5. An individualized treatment plan.
DCMWC will pay for up to a maximum of 60 one-hour treatment sessions during any 90-day period; or a maximum of 90 one-hour sessions during any 12-month period. Lifetime maximums may also apply.
In accordance with 20 CFR 725.707(b), DCMWC may require reports of treatment from time to time, including an individualized treatment plan for each patient.
There is no change in the procedures for billing for other medical services that may be related to pulmonary rehabilitation services. For example, bills for established patient office visits and pulmonary function tests still do not require a Certificate Medical Necessity (CMN) and can be billed separately as they are now. There is also no change in the procedures for prescriptions for durable medical equipment (DME) or home nursing care, which will require a CMN.
All medical bills should be sent to:
DCMWC/Federal Black Lung Program
P.O. Box 8302
London, KY 40742-8302
DCMWC Announcement: Modernizing Payment of Medical Benefits
Notice of Final Rule
The Office of Workers' Compensation Programs has issued a Final Rule governing the Black Lung Disability Trust Fund's payment of medical benefits under the Black Lung Benefits Act. The Final Rule:
- Adopts modern payment formulas for physicians, hospitals and other providers that are derived from the formulas used in the Medicare program. These formulas are also similar to those used by other OWCP programs (e.g., Federal Employees Compensation and Energy Employees Occupational Illness Compensation programs).
- Codifies the black lung program's current practices for the payment of prescription drugs and the submission of medical bills for payment.
- Provides greater clarity about fees paid to providers, which should speed processing and payment of benefits as well as make it easier for the Trust Fund to obtain reimbursement from coal companies.
- Prohibits providers from seeking additional payments from miners for covered services that have been paid by the Trust Fund.
Miners will not see any change in the medical care they receive to treat their black lung disease.
The regulations will be effective August 31, 2018. The rules will apply to medical equipment, prescription drugs, and inpatient medical services provided or rendered after that date. The rules governing payment of professional medical services and outpatient medical services have a delayed application date and will apply to services rendered after April 27, 2020.
The Final Rule is available for public inspection today on the Federal Register's website at: https://www.federalregister.gov/documents/2018/06/14/2018-12418/black-lung-benefits-act-medical-benefit-payments. The Federal Register published the rule on June 14, 2018. The published version is available online at the same website location.
DCMWC Announcement: Final Rulemaking on Medical Benefit Payments
On June 14, 2018, the Office of Workers' Compensation Programs Division of Coal Mine Workers' Compensation issued a final rule governing the Black Lung Disability Trust Fund's payment of medical benefits under the Black Lung Benefits Act. The revised regulations became effective on August 31, 2018. Most of them, including those governing payments for medical equipment, prescription drugs, and inpatient medical services, applied immediately. However, the regulations governing payment of professional medical services and outpatient medical services had a later applicability date of November 30, 2019, so that a new computer system could be developed to process these bills. OWCP is delaying the applicability date of the regulations governing payments for professional medical services and hospital outpatient services from November 30, 2019, to April 26, 2020, due to unforeseen delays in developing the computer system. More information is available at: https://www.dol.gov/owcp/dcmwc/
